Did you know that some mothers might experience postpartum conditions such as Diastasis Recti and Incontinence? You may have never heard of these conditions, or you may have experienced them but do not consider them dire to fix. However, these are two of the more common postpartum conditions that mothers should be aware of, especially with multiple pregnancies. These conditions do not always appear to be life-threatening but they may interfere with your daily life and routine. We understand the struggles of motherhood and its accompanying postpartum related conditions, so here we are to help.
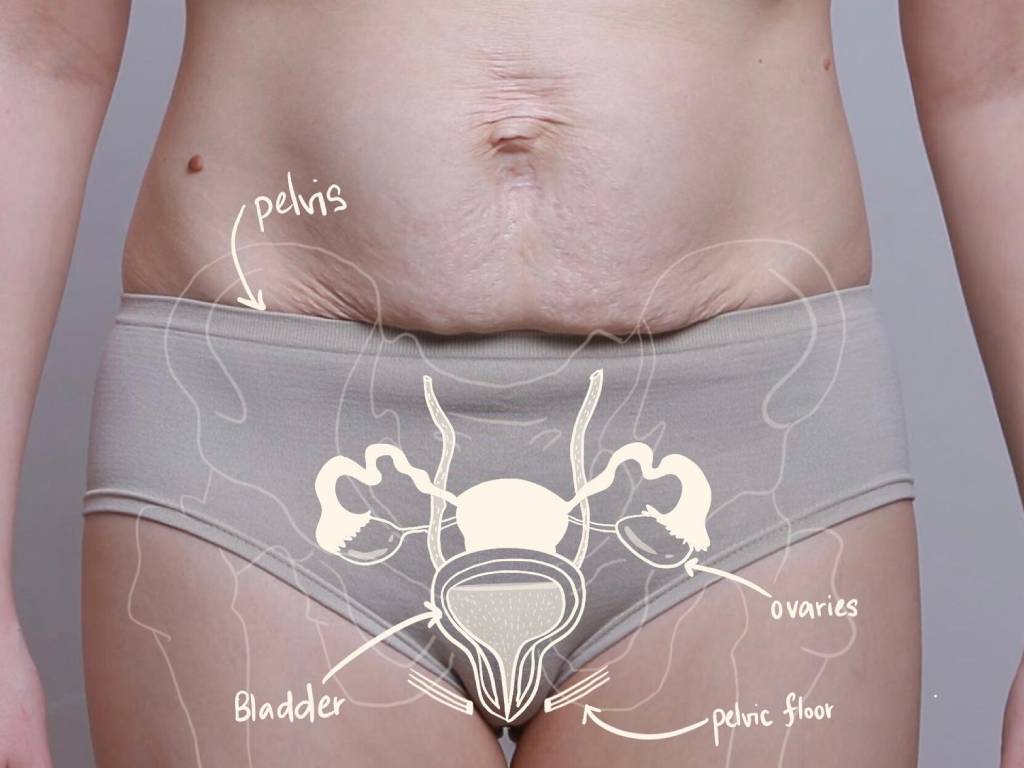
Diastasis Recti Abdominis (DRA) refers to a separation wider than 2.7cm between the left and right rectus abdominis muscles. Around 80% of women develop DRA in the third trimester of pregnancy and 50% continue to have this condition after childbirth. Urinary Incontinence refers to an involuntary urinary leakage marked by a loss of bladder control. Although it is a condition that anyone may develop, It is a condition that could affect anyone but ‘females are twice as likely to suffer from incontinence than males.’ (Davis, 2008). This is attributed to several factors such as pregnancy, childbirth and hormonal changes during menopause.
Many women are vulnerable to these two conditions – Diastasis Recti Abdominis happens in ‘1 in 2 women post-pregnancy’ (Colleen, 2020) and a mother’s risk of developing Incontinence increases with natural birth.
With a focus on Incontinence and Diastasis Recti, the aim of this article is to educate mothers on:
(1) The causes and symptoms of these conditions, and
(2) How to manage them.
Along with this is a self-assessment quiz that would estimate which stages of the conditions you are at. At Orchard Clinic, mothers receive a treatment plan customised to their postpartum conditions, and the quiz results would provide a possible outline of how yours would look.
In this trying and stressful period of the COVID-19 Pandemic, we understand how difficult it is to balance time between your loved ones, motherhood and your well-being. It may be too time-consuming to come down and book an appointment only to realise that your postpartum condition could be inconclusive.
To save time, we have designed a self-assessment quiz that may determine the severity of your condition for Diastasis Recti Abdominis or Incontinence. Thus, from there, your results will be emailed to you along with further information about your condition and a recommended treatment plan (if suitable).
Take the quiz now for Diastasis Recti Abdominis (DRA) and Incontinence.
Wondering what are the risk factors and ways to prevent the conditions from worsening? Read on to find out and click the links to learn more. To read more into depth about these two conditions, you may click on the title of each condition.

Diastasis Recti Abdominis (DRA)
Risk Factors
DRA is caused by the stretching of a connective collagen sheath with excessive inner-abdominal pressure. It most frequently occurs in pregnant or postpartum women. You may be at risk of having DRA if you have/had:
- A larger baby, twins or a large amount of amniotic fluid
- Multiple childbirths
- Pregnant over the age of 35
- Intense pushing and improper breathing during childbirth
- Weak pre-pregnancy abdominal muscles
- Overuse of abdominal muscles during the third trimester
- Obesity
How Does DR Occur?
When pregnant and understanding DRA, the rectus abdominis, commonly known as the six-pack muscle, has a fibrous cord and connective tissue running down the centre called the Linea Alba. Pregnancy simultaneously stretches the abdominal muscles to accommodate the growing baby while releasing hormones to loosen these connective tissues. The combinative forces frequently weaken and separate the rectus abdominis muscles, resulting in a widening of the centre cord, giving the appearance of a pooch or a “mummy tummy”.
What Will Happen If I Do Not Treat My DR?
What are the complications of an untreated DRA? The rectus abdominis is a key member of the abdominal muscle team. Having a diastasis can affect healthy bodily functions and risk conditions such as:
- Back pain, particularly in the lumbar region.
- Difficult vaginal delivery
- Constipation
- Decreased stability of the pelvis and trunk resulting in other conditions such as:
- Pelvic pain
- Pelvic organ prolapse
- Urinary incontinence
- Hernia (Severe cases)
How And When Should I Treat My DR?
While you may feel helpless and frightened along the postpartum journey, do note that recovery is not always impossible. The natural self-resolution period for DRA is about the first 8 weeks postpartum. If symptoms persist, you will likely have to seek professional intervention. To treat DRA, the core must be retrained to their optimal lines of performance such that the body can regain its healthy coordination. If you want to avoid the condition, it is central to stabilise and strengthen the muscles early. This will mitigate the risks of development or further debilitation of a potential DRA.
Q: What muscles should I be strengthening on my own?
A: Our abdominal muscles can be classified into four main groups. These include:
- Rectus Abdominis
- External Oblique
- Internal Oblique
- Transverse Abdominis
Of these muscles, the transverse abdominis (TVA) is the deepest abdominal layer and can be imagined as the body’s internal corset.

Because the TVA pulls the rectus abdominis together, it is the most critical muscle layer to a successful DRA recovery. Until their stretched soft tissues heal, working the other three muscles should be secondary to the TVA. As such, avoid straining these abdominal muscles as it will only pull muscles further apart at the centre.
These include actions such as:
- Heavy lifting
- Constipation
- Oblique and straight crunches
- Sit-ups
- Leg lowering exercises
- Plank-type position
Urinary Incontinence refers to involuntary urinary leakage and a loss of bladder control.
For women, common causes include:
- Pregnancy,
- Childbirth (especially vaginal births), and
- Hormonal changes during menopause.
Among men, factors that contribute to incontinence include:
- Ageing,
- Hormonal changes,
- Surgery,
- Repeated stress to the pelvic floor through chronic issues such as cough or constipation, and
- Prostate-related issues.
Signs of incontinence can include:
- Loss of bladder control
- Urinary overflow
- Urinary leakage during physical exertion.
- Frequent urges to visit the bathroom, yet do not have much urine to pass.
Often, Incontinence occurs when the pelvic floor muscles are weakened to the point they are no longer able to control and support the bladder and sphincter.
How Long Should Incontinence Last?
Incontinence could be:
- Temporary and caused by everyday habits, or
- Persistent due to underlying medical conditions or physical problems and a weakened pelvic floor.
Temporary Incontinence
- Diuretics such as certain drinks (eg. alcohol, caffeine, carbonated drinks), foods (eg. chocolate, foods high in acidity such as citrus or spicy foods) and medications (eg. heart and blood pressure medications, large doses of Vitamin C) may stimulate your bladder and increase your volume of urine. Urinary incontinence may also be caused by medical conditions (eg. Urinary tract infection (UTI)).
Persistent Incontinence
- Factors such as pregnancy, childbirth, pelvic organ prolapse, age, menopause, hysterectomy, enlarged prostate or prostate cancer can increase your risk as well.
What are the Risk Factors for Incontinence?
- Gender
- Women are more likely to have stress incontinence due to pregnancy, childbirth and menopause. However, men with prostate-related conditions are at greater risk of urge and overflow incontinence.
- Age
- Age and weakened muscles reduce how much your bladder can hold and increase the chances of involuntary urine release.
- Being overweight
- Additional weight increases pressure on the bladder and pelvic floor, weakening the muscles and often causes stress urinary incontinence (SUI).
- Other diseases
- Neurological disease or diabetes may increase your risk of incontinence.
Tips to Managing Your Risk of Developing Incontinence
- Maintain a healthy weight
- Practice pelvic floor exercises
- Avoid bladder irritants, such as caffeine, alcohol and acidic foods
- Eat more fibre, which can prevent constipation, a cause of urinary incontinence
- Don’t smoke, or seek help to quit smoking
Can I Live With The Condition?
While common, incontinence is not a normal part of the ageing process! Incontinence is also not something you have to live with after giving birth to your baby. The fear of incontinence, whether urinary or faecal, often stops people from doing things they enjoy and drastically affects their quality of life. Seeking early treatment for Incontinence is often more effective with faster results. If left untreated, Incontinence may worsen with time and even result in a pelvic organ prolapse in very severe cases.
How Does Orchard Clinic Treat These Postpartum Conditions?
- Diastasis Recti Abdominis (DRA)
The only way to treat a DR (besides surgery) is to re-establish the Core team muscles (ie. The Diaphragm, Pelvic floor, TVA and Deep back muscles). Traditionally, they were strengthened through physical exercises. However, these efforts often met with limited success due to reasons such as:
- The amount of time and discipline required
- The duration it takes to see results
- Lack of muscle awareness
This is especially so for mothers suffering from a DRA of a width wider than 4.0CM, physical exercises were often too tedious for their levels of returns. Therefore, to recover mothers in the shortest time possible, Orchard Clinic combines physical exercise with the latest technologies to rapidly accelerate recovery, and offer treatments with the highest level of intensity.
By focusing electromagnetic energy on the treatment area, High Intensity Focused Electromagnetic Therapy enables supramaximal contractions that effectively re-educate the muscles and form healthier muscle memory. Our proven DR treatment stimulates 20,000 contractions in the abdominal muscles, a high level of intensity and repetition that is impossible without the use of medical devices so that tissues in the body can safely and quickly be restored to their lines of optimal functionality.
Core-specific exercises are very effective in reducing DRA, but did you know that not all exercises can be performed with a DR? Therefore, Orchard Clinic offers supervised floorwork sessions for both DRA and Pelvic Floor issues. Sequences are specially tailored to the needs of patients with DR or pelvic floor concerns, and with progressive levels of intensity. Research has shown that in the antenatal period, DRA can be reduced by 35% through core-specific exercises. Thus, having a core-specific program during both the ante and postnatal periods may also reduce DRA width.
2. Incontinence
Orchard Clinic applies the same proven method to the treatment of Incontinence, except this time, we focus on the Pelvic Floor Muscles!
FDA approved Emsella device uses HIFEM technology to enable over 11,000 supramaximal pelvic floor muscle contractions. This is physically impossible and helps significantly to re-educate the muscles and create greater muscle memory.
Exilis Ultra Femme 360 provides the fastest non-invasive radiofrequency treatment for the female intimate area.
This procedure is ideal for women who:
- Suffer from Stress Incontinence,
- Struggle with the appearance of their vagina and the surrounding area, or
- Are looking for non-surgical improvement of their intimate health.
Utilising Ultrasound and Radiofrequency, this safe and comfortable treatment can be used to treat both the internal and external vaginal tissues.
Focuses on the pelvic floor muscles which are responsible for a variety of functions. These muscles support the pelvic organs, assist in bowel and bladder control, and contribute to sexual function and satisfaction. Our programme is specially tailored to the needs of patients with pelvic floor or chronic pain concerns, by addressing the unique challenges that present in the later stages of the rehabilitation process.

Are You Suffering From Other Postpartum Conditions Not Mentioned Above?
Mothers also suffer from many other common conditions such as:
- Skin Laxity,
- Pelvic Pain & Tightness,
- Pelvic Organ Prolapse,
- Menopause and Vaginal Laxity
Do check out the list of conditions we treat and a list of Frequently Asked Questions (FAQs) for more information about such conditions.
Orchard
302 Orchard Road, Tong Building
#06-03 Singapore 238862
| Mon, Wed, Fri, Sat | 9:00AM – 6:00PM |
| Tue & Thu | 9:00AM – 8:00PM |
| Sun & PH | Closed |
Parkway Parade
80 Marine Parade Road, Parkway Parade Office Tower
#08-04 Singapore 449269
| Mon, Wed, Thu, Fri, Sat | 9:00AM – 6:00PM |
| Tue | 9:00AM – 8:00PM |
| Sun & PH | Closed |
Bukit Timah
1 Fifth Avenue, Guthrie House
#02-04 Singapore 268802
By Appointment Only
Copyright © 2024 Orchard Clinic. All Rights Reserved. Privacy Policy | Sitemap